Hypospadias
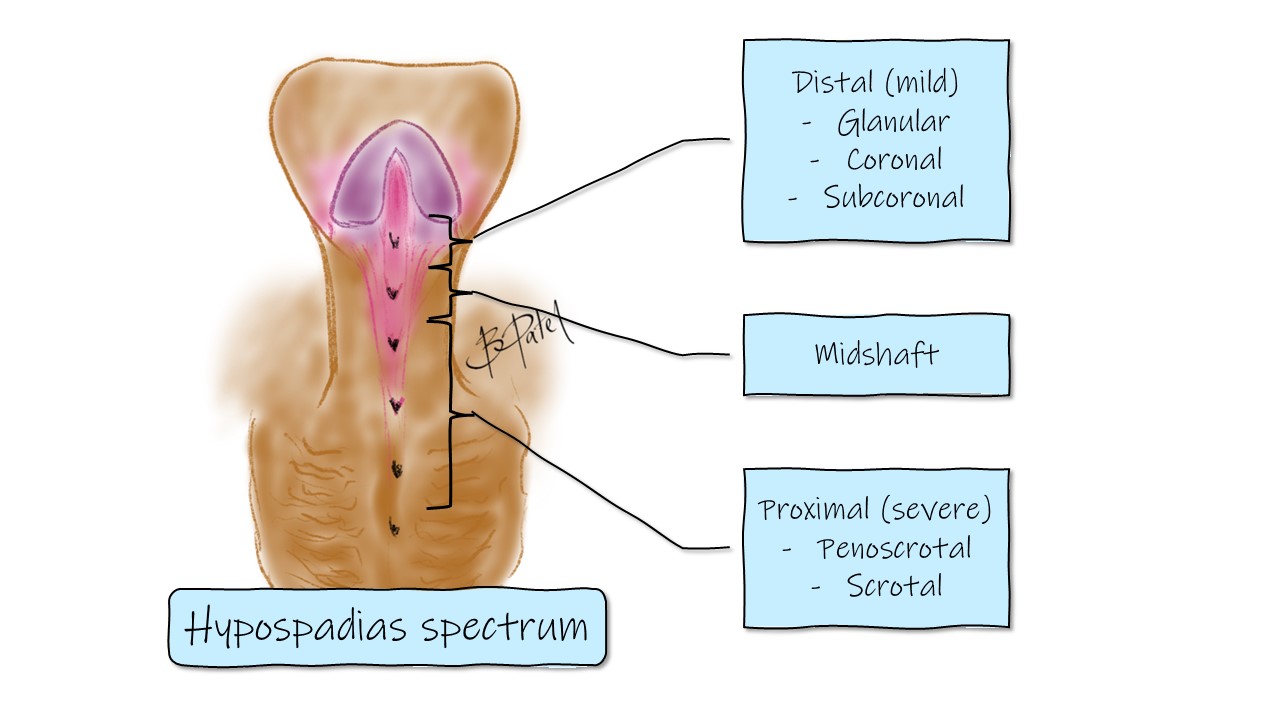
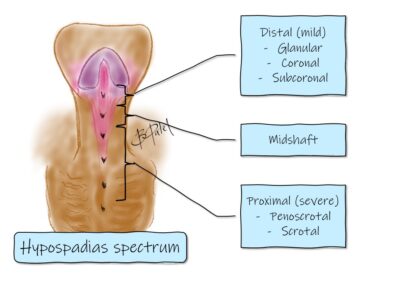
A condition where the urinary opening of the male penis is on the undersurface of the shaft rather than the tip. There is quite a spectrum of issues in this area.
The Condition
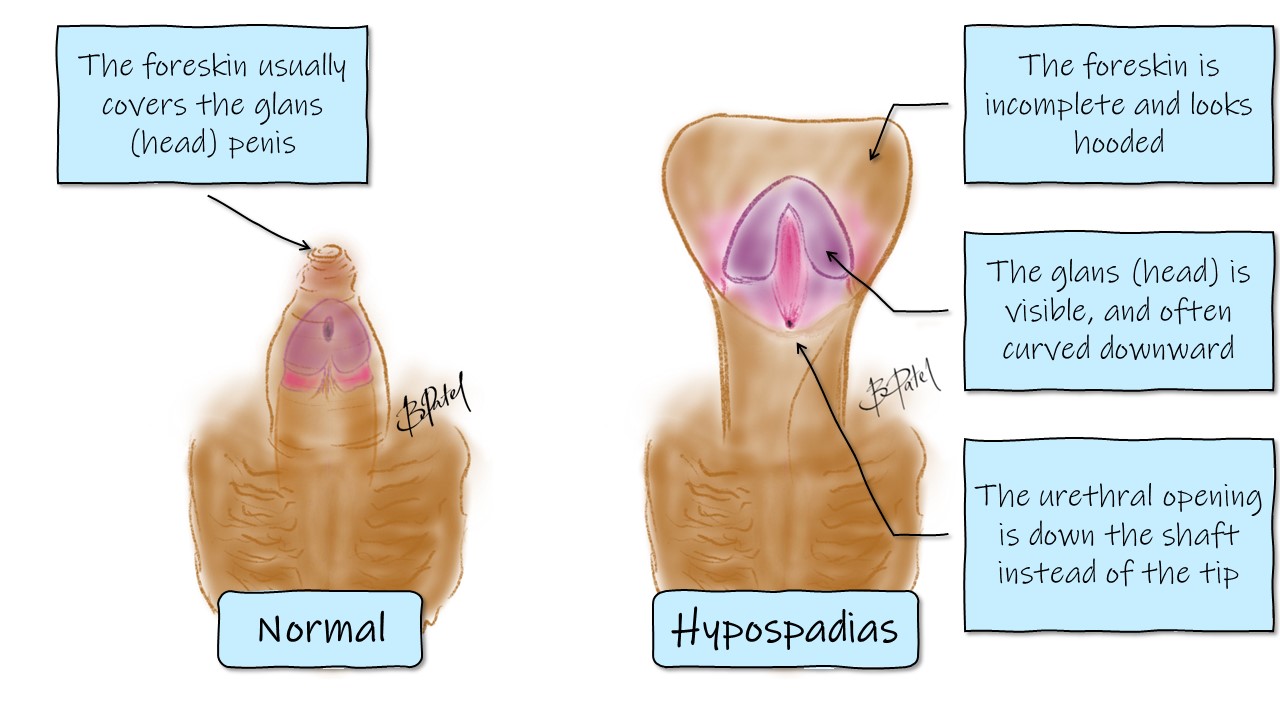
What is hypospadias
A condition usually describing a developmental problem of the male penis. It occurs in about 1 in 200 boys. There are 4 main features that exist on a spectrum:
- The urethra (urinary opening) is found down on the shaft rather than the tip. The urinary stream is usually diverted downward.
- The shaft is often curved forward or downward. This is called chordee (pronounced KOR-dee)
- The foreskin has a hooded appearance as it doesn’t completely cover the head of the penis.
- The glans (head of the penis) is visible, because the foreskin doesn’t cover it.
Why does it occur?
There is no unifying cause of hypospadias. It is more common in boys conceived with in-vitro fertilisation (IVF) techniques, and therefore likely have a hormonal influence. Usually the condition occurs spontaneously, and are seen more frequently if there is a family history. It can occur with other conditions or syndromes such as those associated with genital development problems or chromosomal abnormalities.
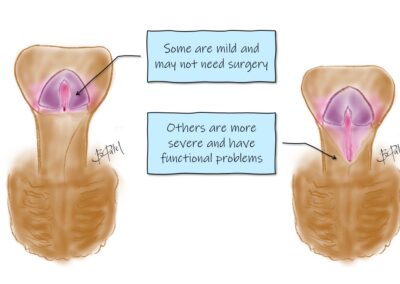
Does it need repair?
Not always and not urgently. In boys with mild hypospadias, repair may not be necessary. For boys with a urinary opening that is clearly abnormal, associated with a penile curve more than 20 degrees, an operation is usually beneficial.
Examination needs to be done by a surgeon experienced with this condition, as initial appearances may be deceiving.
The main focus of repair is to have better function as described below:
- Straight shaft and controllable urinary stream
- Adult function (eg. sexual intercourse)
- Psychological well-being
The goal of surgery for hypospadias is to straighten the shaft, provide a controllable straight urinary stream, normalise the appearance of the penis and prevent any future psychological issues related to the function and appearance of the penis.
What is chordee?
This is the forward curvature of the penis. You will notice the shaft is bent forward. This is part of the spectrum of hypospadias issues. Sometimes there is just a curvature, and the rest is fine. Depending on how much curvature there is, an operation may still be worthwhile. Usually we would consider correction of chordee if the curvature is more than 20 degrees.
What about circumcision?
How do you pronounce hypospadias?
The word “hypospadias” is pronounced as hi-puh-SPAY-dee-uhs.
It comes from Greek – “hypo” = under or below, “spadon” = opening.
Here’s a breakdown of the syllables:
1. “hi” – pronounced like the word “high” without the “gh” sound.
2. “puh” – pronounced as it appears, with a short “uh” sound.
3. “SPAY” – pronounced like the word “spay,” with emphasis on the “ay” sound.
4. “dee” – pronounced like the letter “D.”
5. “uhs” – pronounced like the plural of the letter “U,” followed by the “s” sound.
Putting it all together: hi-puh-SPAY-dee-uhs.
Treatment
Surgical repair
The operation is done under general anaesthetic as a day procedure (you’ll be able to go home the same day). For severe cases or multi staged repairs it may be necessary to stay overnight.
The type of procedure varies depending on the anatomy and examination under the anaesthetic. The end of the penis is reconstructed to position the opening near the tip, the forward curvature (chordee) is corrected, and the skin covers the shaft to either reconstruct the foreskin or circumcise the penis.
A catheter or stent (a tube) is placed to allow healing of the repair. This drains urine from the bladder and sits in a second outer nappy. The catheter is manageable at home and is removed between 3 and 10 days depending on the type of repair.
In more severe cases, the reconstruction requires more than 1 operation. Your surgeon will discuss with you in more detail.
How long does the operation take?
The operation takes about 1-2 hours.
The anaesthetic can take at least half an hour before and after so you’ll be away from your child for a few hours until they are ready for you in the recovery room. You will be notified when they are ready for you to see them in recovery.
When should the repair be done?
There are a few time points to consider repair.
It is often easier to repair before toilet training, as it can be difficult to go through toilet training if the area is painful.
The next time point is just before school, where he has good control of the bladder, and we need to make sure the stream is controllable and doesn’t make a mess. Often there is comparison amongst peers, so we want to ensure he feels psychologically ready to deal with potential differences.
Any time older is acceptable, although it can be a difficult process to have the repair during teen years due to strong uncontrollable erections, and perhaps more sensitivity.
What are the risks of the operation?
- The anaesthetic – airway and breathing issues are extremely rare.
- There are standard risks of any operation. These include bleeding and bruising and wound healing problems such as infection. A scar always develops, although is fairly hidden due to the methods used.
- About 25-30% require another procedure. The repair sometimes doesn’t heal well and a leak from the sutureline may develop (called a fistula). This is usually repaired a few months after, or sometimes it’s safer to wait until toilet training is complete to repair under better control. The repair of the glans (head of the penis) can sometimes become narrow (stenosis), requiring a small procedure to widen the opening. There can be minor issues such as skin irregularities that require more of a cosmetic correction.
- Problems are more likely to occur in the first 2 years after surgery, or around puberty as the penis grows larger. The scarring may not stretch, resulting in curvature issues or a leak (fistula).
Anaesthetic options
There are some options for pain relief at the time of the operation. Once asleep, we can either place local anaesthetic to numb the area just around the penis (called a penile nerve block), or place it into the back, like an epidural block. This is called a caudal anaesthetic. Either way, your child will be completely asleep under the anaesthetic and won’t feel it. The anaesthetist will give you options and you can choose which technique you are most comfortable with using for your child.
Recovery
What happens after the operation?
Recovery – you will be called into the recovery room just after they are awake.
Feeding – you can feed in the recovery room.
Home – usually after a few hours, once the nursing team have ensured your child is safe, comfortable, and you have been shown how to use the double nappy technique and care for the catheter.
Nappy changes will require more than 1 person, to keep his hands off the area. We need to keep his hands away / occupied for a few months afterwards to prevent injury and breakdown of the repair.
Follow up – review / change of dressings around 3-5 days, removal of catheter around 5-10 days. Ongoing review is usually 6 weeks to 3 months, and 1 year afterwards. If all is well, no further review is required unless there are concerns.
The Wound / Dressings
The area will become swollen and bruised.
Nappy changes will require more than 1 person to keep his hands away from the area.
We need to keep his hands away / occupied for a few months afterwards to prevent injury and breakdown of the repair.
You will be shown how to look after the catheter, and place it in double nappies.
Despite this, sometimes the area becomes soiled in a dirty nappy and may need a change (or removal) of the dressing in the emergency department.
Please ensure you have some barrier cream / vaseline to apply to the area to prevent the nappy from sticking to the wound. This can be applied to the inside of the nappy, or directly on the penis. This also helps with itchiness after surgery.
Your surgeon will make plans for the dressing review and catheter removal in the first week after the operation.
Pain relief
Your child will receive good pain relief in the operating room, that will last a few hours.
After the operation they will need paracetamol and possibly ibuprofen (eg. Nurofen) for a few days. Please let your surgeon and anaesthetist know if your child has intolerances or allergies.
In order to avoid medication, aim to distract your child and keep their mind off the area.
Normal activity
Bath / shower – If a catheter is in place, then sponge bath. Once it is removed, can bathe / shower normally. If a catheter wasn’t used, then bathe / shower the day after surgery.
Swimming – can resume after the catheter is out, and the wound looks clean. This is usually 1 week after surgery.
Daycare / School – usually 1-2 weeks.
Sports – older boys will need 2-3 weeks off sports.
Troubleshooting
The dressing is soiled after bowel movement
This is common. Most of the time, it can be cleaned with wet wipes, and occasionally you may need to come back to the emergency department for change of dressing. Depending on the timing after surgery, the dressing may be removed.
Is there an infection? The wound is oozing, and it is very swollen.
Infections can develop around 2-4 days after the operation, and is a fairly uncommon issue. He would have been given antibiotics during the operation and a prescription to take some more antibiotics every night while the catheter is in.
Wound ooze is also common, as the swelling settles. Often it can be blood stained too.
Swelling is expected, to quite a large degree. This will settle after a few weeks.
The wound may be infected if there is increasing redness around the wound and tenderness. This may be associated with discharge from the wound site.
You will need to see your family doctor or call your surgeon for further advice.
He is passing blood
This is quite common. The catheter often irritates the bladder, making the urine look a little red, like cordial. The wound can also ooze, which looks a similar red colour. This will settle in time.
If you see it leaking around the dressing, with clots, or if you are worried about excessive bleeding, please proceed to the emergency department. Don’t feed, just in case he needs an empty stomach for sedation.
What do I look for?
You know your child best. If you have any concerns please see your family doctor or call your surgeon. The list below are issues that require medical attention.
- Increasing pain or persisting pain despite pain relief
- Increasing swelling or bulge after the catheter is removed.
- Fever >38.2 degrees Celsius
- Vomiting and reduced oral intake. (It is ok to lose appetite for a few days, as long as he is getting enough).
- Discharge or bleeding from the wound
- No bowel motions after 3 days – he may need some laxatives.
- Observe the urinary stream. Is it straight, spraying or double? You can take a video and bring it to the appointment.
He has a double stream. Does he have a fistula?
This happens in about 10-20% of boys having this repair, much higher if it is a proximal repair. The urine has found a way out through the sutures. There may be a drip or a double stream.
It can occur in the first 2 years after repair, or around pubertal development as the shaft grows.
Your surgeon will discuss options and repair.
Experienced Surgeons
Over 25 years experience in paediatric surgery
Locations
Queensland and northern New South Wales
Appointments
Prioritised time for your child
Information
Conditions, procedures and aftercare
In the spirit of reconciliation we acknowledge the Traditional Custodians of country throughout Australia and their connections to land, sea and community. We pay our respect to their Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.