Undescended Testis
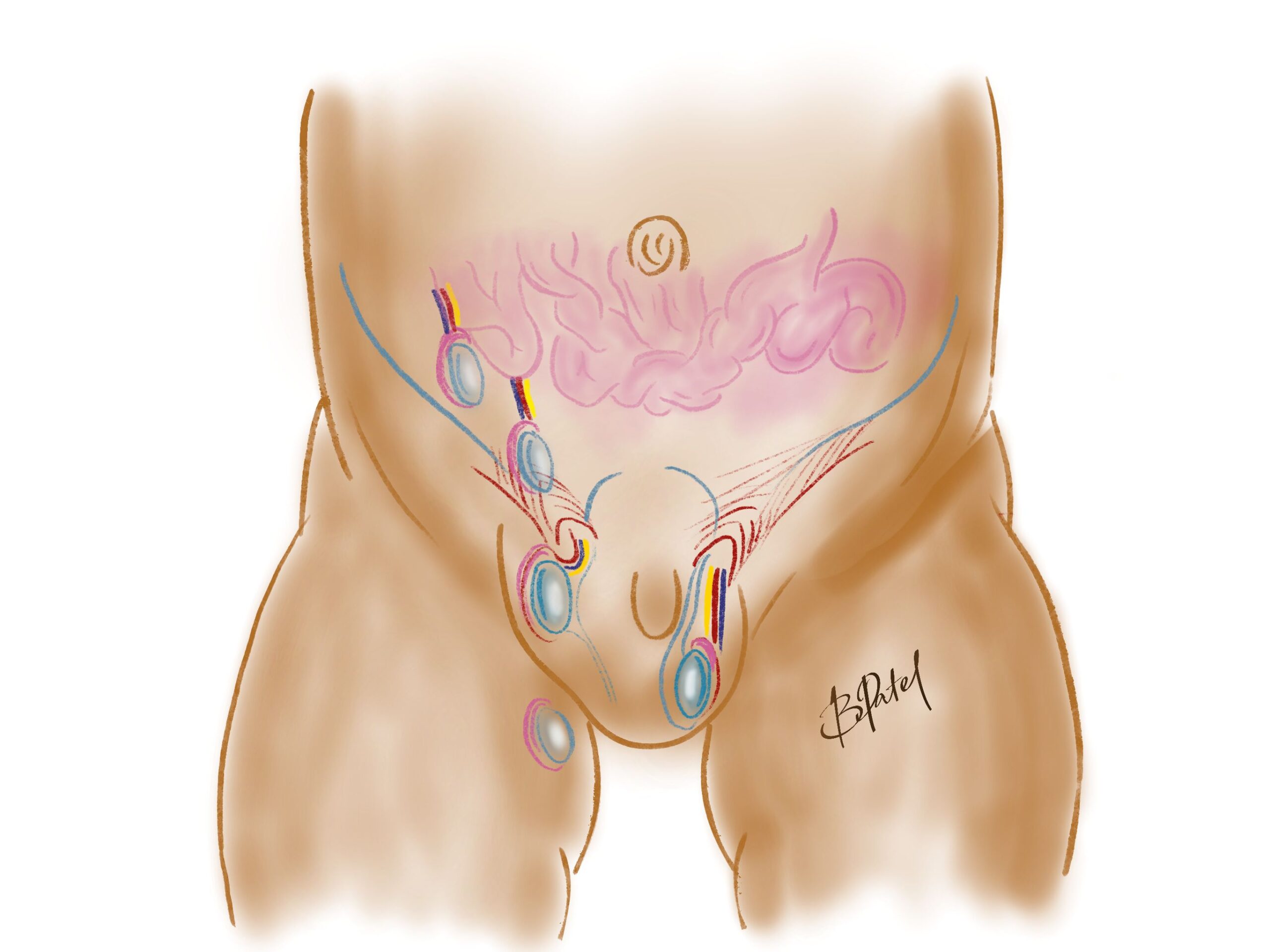
This is a condition where one or both testes (or testicles) do not make their way from the abdomen into the scrotum. An operation called orchidopexy (or orchiopexy) is performed to reposition the testis into the scrotum.
The Condition
What is an undescended testis?
An undescended testis, also known as cryptorchidism, is a condition where one or both of a male infant’s testicles have not moved into their proper position in the scrotum before birth. The testicles normally form in the abdomen during fetal development and gradually descend into the scrotum during the last few months of pregnancy. However, in some cases, this descent does not occur, resulting in an undescended testis.
Cryptorchidism is one of the most common genital abnormalities in male infants, affecting approximately 3-5% of full-term boys and up to 30% of premature infants. While the majority of cases involve only one undescended testicle, some boys may have both testicles undescended.
Why does it occur?
The exact cause of this condition is not always clear. It is likely to be influenced by a combination of genetic, hormonal, and environmental factors.
Risk factors for an undescended testis include premature birth, low birth weight, and a family history of the condition. It can occur as part of a range of conditions, syndromes or chromosomal disorders including those with variations of sexual characteristics (also called ambiguous genitalia, or disorder of sexual differentiation).
Does it need repair?
The testes work best when in the scrotum, to be at a slightly lower temperature than the rest of the body. The main reasons for treatment relate to fertility and cancer risk.
The risk of cancer in the testes is estimated at 1 in 100,000. There is a slightly higher risk of malignancy (cancer) with undescended testes. By bringing the testes into the scrotum, there is a better ability to detect any abnormality as early as possible. Boys must be taught to perform self examination during their teens to help detect any lumps as they grow into adults.
An undescended testis is also at higher risk of torsion (twisting) and becoming damaged. Repair can help prevent this risk.
Fertility may be affected by the abnormal position of the testis. A boy with both undescended testes can have reduced fertility.
If the testes haven’t descended by 6 months then an operation is worthwhile to mobilise it into the scrotum. This is done by performing surgery, called orchidopexy or orchiopexy.
Is it dangerous?
One main concern is that it can affect fertility because the testicle needs to be in the scrotum where it is cooler, which is important for making healthy sperm.
There is also a higher risk of developing testicular cancer later in life if the testis stays undescended. Other issues could include testicular torsion, where the testicle twists and cuts off its own blood supply, and inguinal hernia, where a part of the intestine bulges into the groin area.
To prevent these problems, it’s important to get medical advice early and follow the recommended treatments. Early action can help ensure your child’s long-term health and well-being.
How is it diagnosed?
Diagnosing an undescended testis usually starts with a physical examination. This usually occurs at the newborn check and 6 week checks.
The clinician will feel the baby’s scrotum and groin area to check if both testicles are in place.
An ultrasound is not recommended, in fact, most ultrasound scans are incorrect, due to normal retractility of the testes. This means it is normal for the testes to move up to the groin and back down to the scrotum.
If you are concerned, please see your family doctor, and if there are ongoing concerns, a paediatric surgeon will need to see your child.
What is a retractile testis?
It is the normal movement of the testis from the scrotum to the groin and back.
There is a muscle in the groin that controls the position of the testis. When its cold, the testis is pulled up into the groin, and when warm the muscle relaxes to allow the testis to descend further.
A retractile testis is considered normal when the muscle relaxes and the testis sits within the scrotum. With activity or even being nervous, the testes are often pulled up by the muscle. This is a normal response.
An ascending testis is one that rises over time, as the boy grows taller. This can take years to diagnose, and often the reason for ongoing reviews over the first few years of life.
Treatment
Surgery (Orchiopexy / Orchidopexy)
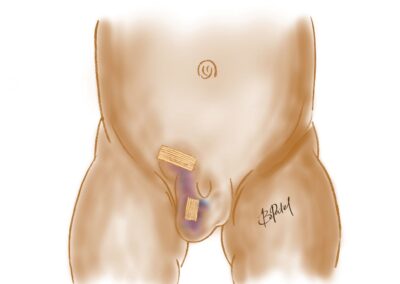
The operation is called orchidopexy (or orchiopexy). This is usually performed after 6 months age as a day procedure under general anaesthetic, through a small incision in the groin and scrotum.
If the testis cannot be felt in the groin, laparoscopy (keyhole surgery) is performed to locate the testis within the abdomen. Because the testis is too high to be brought down in 1 operation, a second operation will need to be performed 3-6 months later to give a better chance for a successful operation.
Occasionally the testis has not formed correctly, and may have had an accident during development. In this case the remnant of the testis is removed, and we will discuss fixation of the good testis.
How long does the operation take?
The operation takes about 20 minutes.
The anaesthetic can take about the same time before and after, so you’ll be away from your child for an hour or so, until they are ready for you in the recovery room.
You will be notified when they are ready for you to see them in recovery.
Timing of surgery
Orchidopexy is recommended around 6-18 months age.
This allows the testes to be positioned in the scrotum, while the child is still in nappies. Anaesthetic risk is also minimal at this time for this short procedure.
Risks of surgery
- The anaesthetic – airway and breathing issues are extremely rare
- Recurrence of high testis- about 1% for most children, more often in premature infants.
- Injury to structures – the testicle, blood vessels and the vas deferens may be injured very rarely.
- Infection -1%
- Bleeding, bruising and swelling. Usually minor, and settles after a week.
- If laparoscopy is performed there is a small chance of a hernia developing in the abdominal wounds.
Recovery
What happens after the operation?
Recovery – you will be called into the recovery room just after they are awake.
Feeding – you can give your child a feed in the recovery room.
Home – usually after an hour or 2, once the nursing team have ensured your child is safe and comfortable
The wound / dressings
The area will become swollen, and a little firm under the wound. This is a normal healing process and developing scar.
There is a waterproof dressing in the groin and scrotum that can be removed in the bath after a week. Glue is often placed on the scrotal wound to keep it waterproof inside the nappy.
Pain relief
Your child will receive pain relief in the operating room and local anaesthetic, that will last a few hours.
After the operation they will need paracetamol and possibly ibuprofen (eg. Nurofen) for a few days. Please let your surgeon and anaesthetist know if your child has intolerances or allergies.
In order to avoid medication, aim to distract your child and keep their mind off the area. Reading, writing, playing games and other engaging activities help.
Normal activity
Bath / shower – the day after the operation
Swimming – 1 week
Daycare / School – 5-7 days
Sports – 2-3 weeks
Troubleshooting
What do I look for?
You know your child best. If you have any concerns please see your family doctor or call your surgeon. The list below are issues that require medical attention.
-
-
- Increasing pain or persisting pain despite pain relief
- Fever >38.2 degrees Celsius
- Vomiting and feed intolerance
- Discharge or bleeding from the wound
- No bowel motions after 3 days
-
Is there a wound infection?
Infections can develop around 2-4 days after the operation, and is a fairly uncommon issue.
The wound may be infected if there is increasing redness around the wound and tenderness. This may be associated with discharge from the wound site.
You will need to see your family doctor or call your surgeon for further advice.
It is very swollen
It does become swollen after the operation, usually for a few days.
If your child has increasing pain, tenderness and redness there may be a wound infection, or bruising.
Please see your GP and call your surgeon so your child can be assessed.
Is it still too high?
This is common in the first few months after the operation. There is swelling and thickening of the tissues, and rarely the scar tissue holds the testis up high.
Rarely another operation needs to be done a few years afterwards to bring the testis down again.
Experienced Surgeons
Over 25 years experience in paediatric surgery
Locations
Queensland and northern New South Wales
Appointments
Prioritised time for your child
Information
Conditions, procedures and aftercare
In the spirit of reconciliation we acknowledge the Traditional Custodians of country throughout Australia and their connections to land, sea and community. We pay our respect to their Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples.